USE OF VOLUME-STABLE COLLAGEN MATRIX FOR SOFT TISSUE AUGMENTATION AT TEETH AND DENTAL IMPLANTS SITE
Badalyan K., Posessor A., Stepanyan Z., Levonyan E., Melkumyan I.
Federal State Institution, Central Research Institute of Dental and Maxillofacial Surgery, Russia, Moscow.
Summary.
Objective.
The aim of this clinical report is to demonstrate the capabilities and the results of a porcine collagen matrix application to increase the soft tissue volume in the area of placed implant at 3.1 site and of implant-supported cantilever prosthesis at 3.2 site.
Materials and methods.
Objective.
The aim of this clinical report is to demonstrate the capabilities and the results of a porcine collagen matrix application to increase the soft tissue volume in the area of placed implant at 3.1 site and of implant-supported cantilever prosthesis at 3.2 site.
Materials and methods.
The material of the study was a clinical case of the 35-year-old patient with a diagnosis gingival recession and lateral resorption of the tooth root 3.2. It is known from the anamnesis that 2 years ago an injury was received in this area. The first stage was resection of this tooth and its replantation in order to preserve the parameters of the bone and gingiva. After the bone healing, teeth 3.1, 3.2 were removed, an implant was installed in the area of the missing tooth 3.1, bone and soft tissue augmentation in this area were performed. 3 months after the operation, a crown was installed on the implant 3.1 and a cantilever structure in the area 3.2. 12 months after the operation and prosthetics, no mucosal inflammation or apical migration of the gingival margin were found. The thickness of the gingiva in the area of the installed implant is 2.5 mm, which is 1.5 mm more than the initial thickness of the gum.
Conclusions.
Teeth can be used as a biological matrix to prevent bone atrophy; in order to prevent soft tissue atrophy and bone resorption, providing an inflammation absence, dental implantation should be combined with soft tissue augmentation; use of volume-stable collagen membrane combined with soft tissue graft provides significant increase of soft tissues (gingival increase by 1.5mm at implant site); long-term use of implantsupported cantilever construction at lower jaw incisors site does not lead to gingival recession as long as sufficient bone and soft tissue volume is provided. Key words. Dental implantation, mucosal thickness, collagen matrix, soft tissue grafting.
Conclusions.
Teeth can be used as a biological matrix to prevent bone atrophy; in order to prevent soft tissue atrophy and bone resorption, providing an inflammation absence, dental implantation should be combined with soft tissue augmentation; use of volume-stable collagen membrane combined with soft tissue graft provides significant increase of soft tissues (gingival increase by 1.5mm at implant site); long-term use of implantsupported cantilever construction at lower jaw incisors site does not lead to gingival recession as long as sufficient bone and soft tissue volume is provided. Key words. Dental implantation, mucosal thickness, collagen matrix, soft tissue grafting.
Introduction.
Soft tissue width and thickness deficiency around teeth and implants can compromise the aesthetic, function or survival of teeth and dental implants. [1-7].
The gold standard of soft tissue increase is the connective tissue autograft transplantation due to its good volume maintance and the side effects absence. [8,9]. However, this method has a number of disadvantages such as post-operative pain syndrome and discomfort, limited donor area volume, possible damage of adjacent anatomical structures and high post-operative complications probability [10].
Numerous biomaterials were developed as an alternative to soft tissue augmentation such as allografts, xenografts and synthetic soft tissues substitutes as well. Volume-stable collagen matrices are the most commonly used biomaterials [5,11].
One of the promising methods for soft tissue defects replenishment is use of porcine collagen matrix. Its indications are large surgical intervention, small donor area volume or its absence, autograft low quality, patients with somatic diseases, patients with low pain threshold [12-14].
Materials and methods. T
The gold standard of soft tissue increase is the connective tissue autograft transplantation due to its good volume maintance and the side effects absence. [8,9]. However, this method has a number of disadvantages such as post-operative pain syndrome and discomfort, limited donor area volume, possible damage of adjacent anatomical structures and high post-operative complications probability [10].
Numerous biomaterials were developed as an alternative to soft tissue augmentation such as allografts, xenografts and synthetic soft tissues substitutes as well. Volume-stable collagen matrices are the most commonly used biomaterials [5,11].
One of the promising methods for soft tissue defects replenishment is use of porcine collagen matrix. Its indications are large surgical intervention, small donor area volume or its absence, autograft low quality, patients with somatic diseases, patients with low pain threshold [12-14].
Materials and methods. T
Thirty-five-year-old patient applied to a dental clinic complaining of pain, suppuration and bleeding in frontal region of lower jaw. Anamnesis Morbi: injury was received about two years ago, six months after the injury endodontic treatment of teeth 3.1, 3.2 was performed.
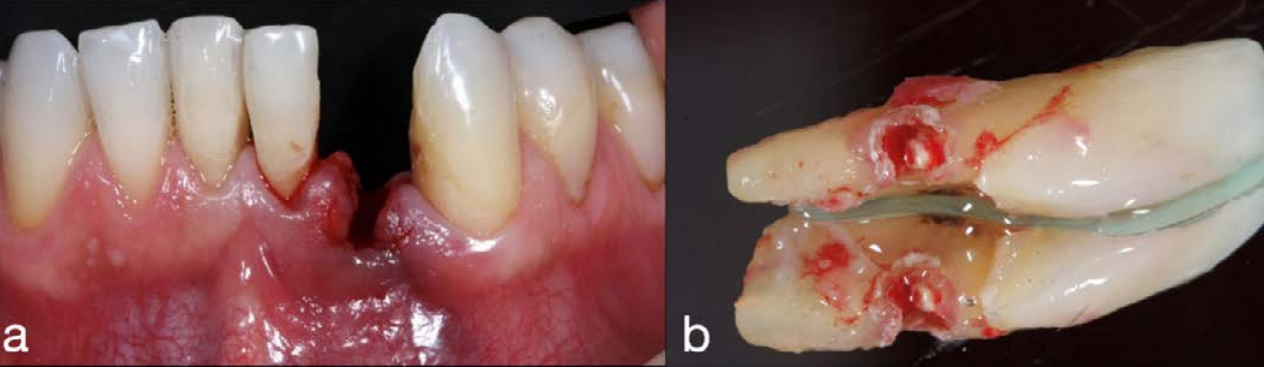
Clinical examination revealed Miller first class recession of tooth 3.2. There was a soft dental plaque accumulation in the lower jaw teeth area. The patient had an average gingival phenotype. The thickness of mucous membrane at the lower jaw incisors site was 1mm (figure 1)/
Clinical examination revealed Miller first class recession of tooth 3.2. There was a soft dental plaque accumulation in the lower jaw teeth area. The patient had an average gingival phenotype. The thickness of mucous membrane at the lower jaw incisors site was 1mm (figure 1)/

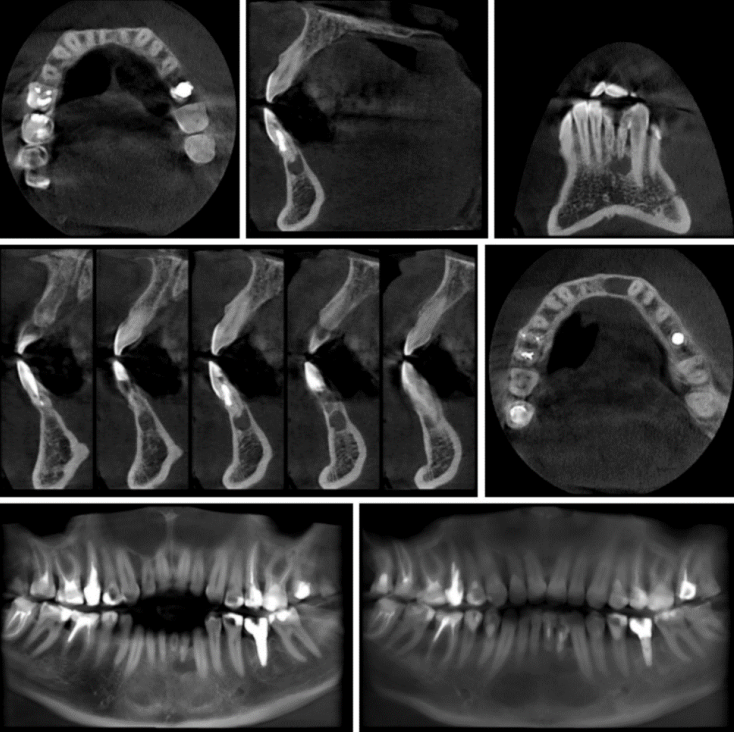
According to CBCT bone tissue destruction in teeth 3.1, 3.2 area and internal lateral resorption of tooth 3.2 root were observed (figure 2).
The treatment involved several stages. Seven days before the first stage of the surgery, oral hygiene was carried out. An informed consent before the treatment was taken. After administration of local anaesthesia with 4% articaine solution (Ubistesin; 3M ESPE) teeth 3.1, 3.2 and root granuloma were extracted (figure 3). After the extraction and clear visualization of tooth 3.2 root’s lateral resorption extraoral resection of extracted teeth roots tips and its retrograde filling using Trioxident material were performed. The resorption cavity of tooth 3.2 root was also sealed.
Then, replantation of teeth 3.1,3.2 and its splinting using composite material were performed in order to restore the bone tissue and to preserve bone alveoli parameters in the lower jaw for subsequent intraosseous dental implantation. For pain control, the patient was prescribed 100 mg of nimesulide (Nise; Dr. Reddy’s Laboratories, India). Post operative period was uneventful (figure 4).

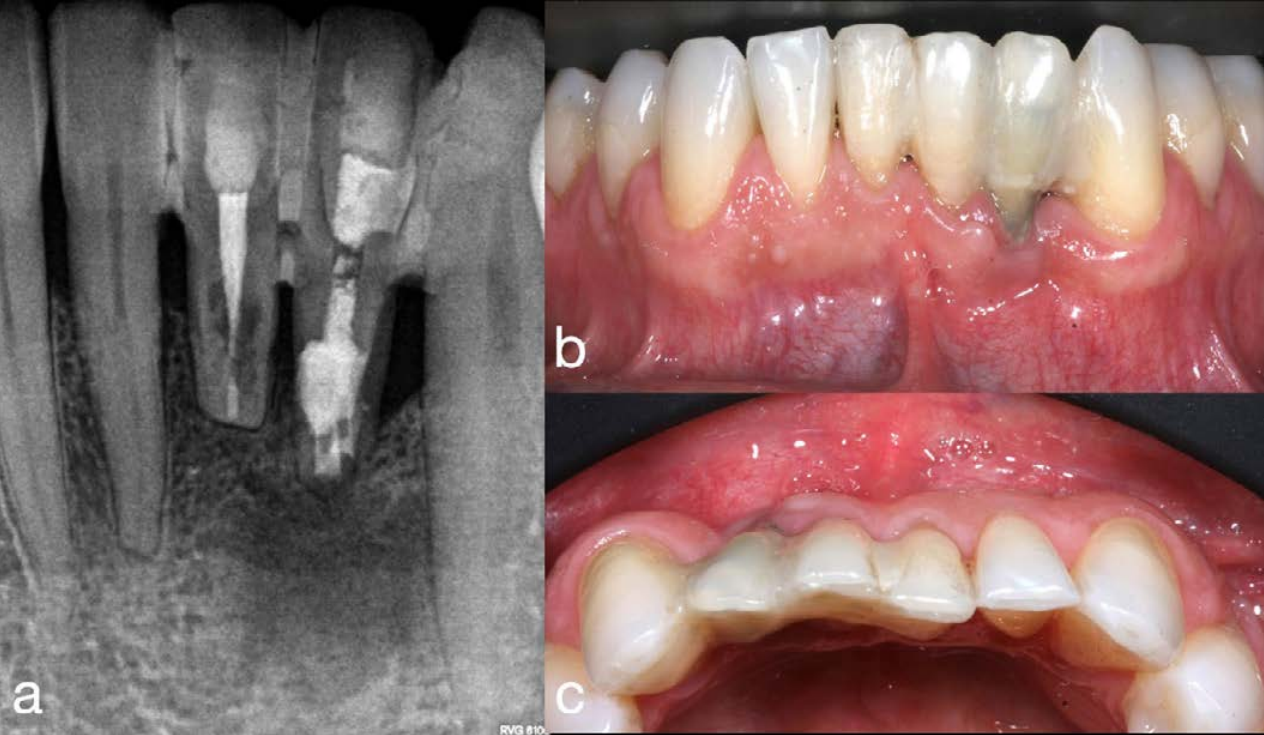
6 months after the extraction and tooth fragment replantation the sighting radiography revealed positive dynamics of bone tissue healing. However, aggravation of soft tissue defect at tooth 3.2 site was observed (figures 5a, 5b, 5c).
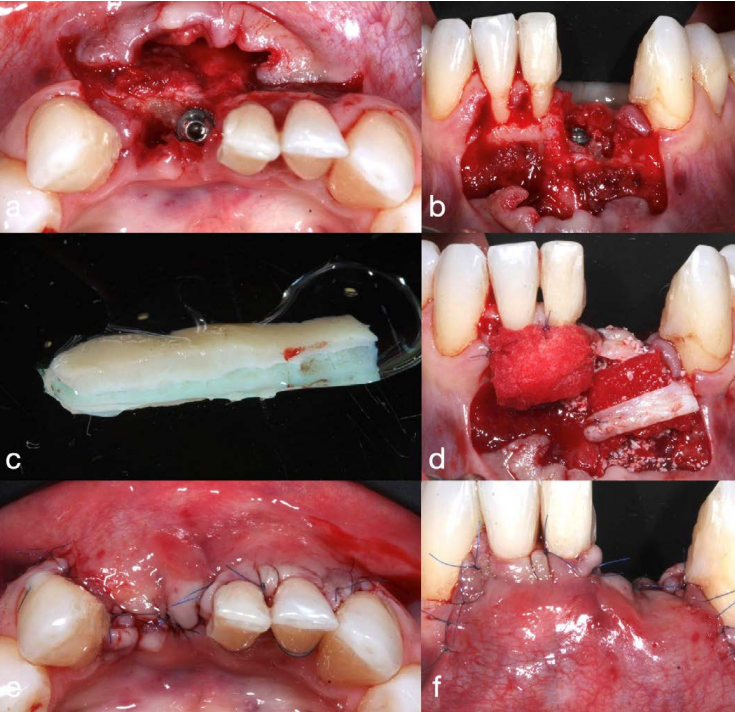
6 months after the extraction and tooth fragment replantation the second surgical stage was conducted. The patient received a prophylactic dose of antibiotic (1 g amoxiclav, Lek d.d, Slovenia) 1 hour prior to surgery. After administration of local anaesthesia with 4% articaine solution (Ubistesin; 3M ESPE) trapezoidal incision of the mucosa at teeth 4.2-3.3 site was performed. Split mucosal flap was elevated. Extraction of teeth 3.1, 3.2 and immediate intraosseous dental implantation at tooth 3.1 site were performed. Astra Tech dental implant (Dentsply sirona) 3.5x11 was installed. A cover screw was installed. Connective tissue graft from the hard palate area was taken and de-epithelized. The thickness of the obtained graft was 1mm. The sockets of extracted teeth were augmented with BioOss osteoplastic material (Geitstlich Pharma AG). Then, volume-stable collagen matrix FibroGide (Geitstlich Pharma AG) previously moistened with saline solution was placed above. The thickness of moisten matrix was 8mm. Matrix was sutured with absorbable Monosyn 6\0 thread on the vestibular side of the defect. Connective tissue graft was sutured above. The flap was mobilized and sutured with Monosyn 6\0 thread without tension. For pain control, the patient was prescribed 100 mg of nimesulide (Nise; Dr. Reddy’s Laboratories, India). 10 days after surgery stitch out and antiseptic treatment of wound surface with chlorhexidine solution 0.2% (Corsodyl, GlaxoSmith- Kline) were carried out. For pain control, the patient was prescribed 100 mg of nimesulide (Nise; Dr. Reddy’s Laboratories, India). Post-operative period was uneventful (figures 6a, 6b, 6c, 6d, 6e, 6f).
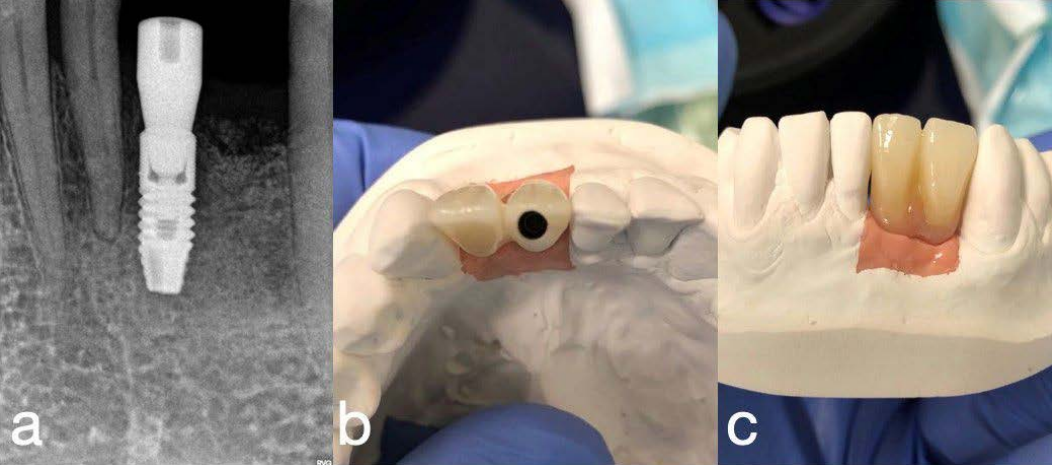
3 months after healing the healing abutment was installed. Prosthetic that included cantilever prosthesis replacing tooth 3.2 and artificial gingiva was made and fixed (figures 7a, 7b, 7c). Control examinations were conducted one week after each surgical stage. Each postoperative period involved soft tissues healing without any features or inflammation signs. Drug treatment included non-steroid anti-inflammatory drugs; antibacterial treatment was not provided.
Results.
1,3,6 and 12 months after the surgery there was no signs of mucous inflammation or gingiva margin apical migration (figure 8a, 8b). 12 months after the surgery the thickness of mucosa at the installed implant site became 2.5 mm which was 1.5 mm more than initial gingiva’s thickness.
1,3,6 and 12 months after the surgery there was no signs of mucous inflammation or gingiva margin apical migration (figure 8a, 8b). 12 months after the surgery the thickness of mucosa at the installed implant site became 2.5 mm which was 1.5 mm more than initial gingiva’s thickness.

Discussion.
Keratinized and attached gingiva volume is one of the main factors of teeth and implants long-term survival. It has a direct influence on bone tissue stability around dental implants as well [7]. Currently, various methods of augmentation with autografts and xenografts are used to increase the thickness of soft tissues. Connective tissue autografts are considered as a gold standard in dental surgery and periodontics for oral cavity tissues deficiency correction [15]. Use of the patient’s own soft tissues is known as reliable and predictable method for ginigiva thickening. However, this method is associated with a few requirements and limitations [16].
One of these limitations is the need to create second surgical site in the donor area which leads to increased pain, postoperative bleeding, increased surgery duration and adds an additional risk of adjacent anatomical structures damage as well [4,17,18].
An important factor is the limited donor area that can be used for soft tissue reconstructions in dental surgery and periodontics.
Thus, a lot of interest has taken place regarding development of autografts substitutes recently. Clinical research revealed that collagen matrices can be used as a connective tissue grafts alternative to soft tissues quality and amount increase [19].
Evaluation of immediate implant placement either using connective tissue grafts, xenografts (Fibro-Gide; Geistlich Pharma AG, Wolhusen, Switzerland) or without soft tissue augmentation was done in retrospective study [1].
The study revealed that soft tissues volume increase is aesthetically and functionally beneficial. Application of porcine xenogeneic collagen matrix (Fibro-Gide; Geistlich Pharma AG, Wolhusen, Switzerland) provides comparable aesthetic and functional results. However, according to visual analogue scale (VAS) it was revealed that patients rated pain by 6.7 points when autografts were used while when using xenografts, the average value was 3.6 points.
Randomized control trial of soft tissue augmentation around dental implants with connective tissue graft and xenogeneic collagen matrix [20] revealed that minimum 2.88 mm of gingival thickness around an implant for a long-term stable implantation outcome is required. The trial also revealed that average gingival growth, following soft tissue augmentation, was 1.33 mm. In our clinical case we achieved soft tissue thickness increase around installed dental implant by 1.4 mm using porcine xenogeneic collagen matrix (Fibro-Gide; Geistlich Pharma AG, Wolhusen, Switzerland). Gingival thickness became equal to 2.5 mm that proves good surgery prognosis.
Stefan Neumeyer published an article where method of bone tissue volume maintaining after tooth extraction using extracted tooth fragments was described [21]. The teeth fragments are formed while segmental cutting of the extracted teeth. These fragments are being replanted and fixed on the extracted tooth socket surface and isolated from mechanical pressure. Tooth segment replantation not only prevents vestibular bone resorption but also provides hard and soft tissues formation. In the presented clinical report, we used fragments of extracted teeth 3.1, 3.2 as a biological matrix to prevent bone and gingival atrophy that allowed us to preserve bone parameters of the ridge and to install an implant without bone augmentation.
Conclusions.
1. Teeth can be used as a biological matrix to prevent bone atrophy. 2. In order to prevent soft tissue atrophy and bone resorption, providing an inflammation absence, dental implantation should be combined with soft tissue augmentation. 3. Use of volume-stable collagen membrane combined with soft tissue graft provides significant increase of soft tissues (gingival increase by 1.5mm at implant site). 4. Long-term use of implant-supported cantilever construction at lower jaw incisors site does not lead to gingival recession as long as sufficient bone and soft tissue volume is provided.
One of these limitations is the need to create second surgical site in the donor area which leads to increased pain, postoperative bleeding, increased surgery duration and adds an additional risk of adjacent anatomical structures damage as well [4,17,18].
An important factor is the limited donor area that can be used for soft tissue reconstructions in dental surgery and periodontics.
Thus, a lot of interest has taken place regarding development of autografts substitutes recently. Clinical research revealed that collagen matrices can be used as a connective tissue grafts alternative to soft tissues quality and amount increase [19].
Evaluation of immediate implant placement either using connective tissue grafts, xenografts (Fibro-Gide; Geistlich Pharma AG, Wolhusen, Switzerland) or without soft tissue augmentation was done in retrospective study [1].
The study revealed that soft tissues volume increase is aesthetically and functionally beneficial. Application of porcine xenogeneic collagen matrix (Fibro-Gide; Geistlich Pharma AG, Wolhusen, Switzerland) provides comparable aesthetic and functional results. However, according to visual analogue scale (VAS) it was revealed that patients rated pain by 6.7 points when autografts were used while when using xenografts, the average value was 3.6 points.
Randomized control trial of soft tissue augmentation around dental implants with connective tissue graft and xenogeneic collagen matrix [20] revealed that minimum 2.88 mm of gingival thickness around an implant for a long-term stable implantation outcome is required. The trial also revealed that average gingival growth, following soft tissue augmentation, was 1.33 mm. In our clinical case we achieved soft tissue thickness increase around installed dental implant by 1.4 mm using porcine xenogeneic collagen matrix (Fibro-Gide; Geistlich Pharma AG, Wolhusen, Switzerland). Gingival thickness became equal to 2.5 mm that proves good surgery prognosis.
Stefan Neumeyer published an article where method of bone tissue volume maintaining after tooth extraction using extracted tooth fragments was described [21]. The teeth fragments are formed while segmental cutting of the extracted teeth. These fragments are being replanted and fixed on the extracted tooth socket surface and isolated from mechanical pressure. Tooth segment replantation not only prevents vestibular bone resorption but also provides hard and soft tissues formation. In the presented clinical report, we used fragments of extracted teeth 3.1, 3.2 as a biological matrix to prevent bone and gingival atrophy that allowed us to preserve bone parameters of the ridge and to install an implant without bone augmentation.
Conclusions.
1. Teeth can be used as a biological matrix to prevent bone atrophy. 2. In order to prevent soft tissue atrophy and bone resorption, providing an inflammation absence, dental implantation should be combined with soft tissue augmentation. 3. Use of volume-stable collagen membrane combined with soft tissue graft provides significant increase of soft tissues (gingival increase by 1.5mm at implant site). 4. Long-term use of implant-supported cantilever construction at lower jaw incisors site does not lead to gingival recession as long as sufficient bone and soft tissue volume is provided.
REFERENCES
1. Angelis P, Manicone PF, Gasparini G, Angelis S, Liguori MG, Filippis I, D'Addona A. Influence of Immediate Implant Placement and Provisionalization with or without Soft Tissue Augmentation on Hard and Soft Tissues in the Esthetic Zone: A One-Year Retrospective Study. Biomed Res Int. 2021;2021:8822804.
2. Ashurko IP, Tarasenko SV, Esayan AV, Galyas AI, Li AV. Evaluation of free connective tissue graft and collagen matrix clinical effectiveness to increase soft tissue thickness around dental implants. Paradontology. 2022;27:2.
3. Bassetti M, Kaufmann R, Salvi GE, Sculean A, Bassetti R. Soft tissue grafting to improve the attached mucosa at dental implants: A review of the literature and proposal of a decision tree. Quintessence Int. 2015;46:499-510.
4. Burkhardt R, Hämmerle CHF, Lang NP, Research Group on Oral Soft Tissue Biology & Wound Healing. Self-reported pain perception of patients after mucosal graft harvesting in the palatal area. J Clin Periodontol. 2015;42:281-287.
5. Caballé-Serrano J, Zhang S, Ferrantino L, Simion M, Chappuis V, Bosshardt DD. Tissue Response to a Porous Collagen Matrix Used for Soft Tissue Augmentation. Materials (Basel). 2019;12:3721.
6. Gargallo-Albiol J, Barootchi S, Tavelli L, Wang HL. Efficacy of Xenogeneic Collagen Matrix to Augment Peri-Implant Soft Tissue Thickness Compared to Autogenous Connective Tissue Graft: A Systematic Review and Meta-Analysis. Int J Oral Maxillofac Implants. 2019;34:1059-1069.
7. Giannobile WV, Jung RE, Schwarz F, Groups of the 2nd Osteology Foundation Consensus Meeting. Evidence-based knowledge on the aesthetics and maintenance of peri-implant soft tissues: Osteology Foundation Consensus Report Part 1-Effects of soft tissue augmentation procedures on the maintenance of peri-implant soft tissue health. Clin Oral Implants Res. 2018;29:7-10.
8. Deo SD, Shetty SK, Kulloli A, Chavan R, Dholakia P, Ligade S, Dharmarajan G. Efficacy of free gingival graft in the treatment of Miller Class I and Class II localized gingival recessions: A systematic review. J Indian Soc Periodontol. 2019;23:93-99.
9. Zucchelli G. и др. Autogenous soft tissue grafting for periodontal and peri-implant plastic surgical reconstruction. J. Periodontol. 2020;91:9-16.
10. De Angelis P, De Angelis S, Passarelli PC, Liguori MG, Pompa G, Papi P, Manicone PF, D'Addona A. Clinical comparison of a xenogeneic collagen matrix versus subepithelial autogenous connective tissue graft for augmentation of soft tissue around implants. Int J Oral Maxillofac Surg. 2021;50:956- 963.
11. Moraschini V, de Almeida DCF, Sartoretto S, Bailly Guimarães H, Chaves Cavalcante I, Diuana Calasans-Maia M. Clinical efficacy of xenogeneic collagen matrix in the treatment of gingival recession: a systematic review and meta-analysis. Acta Odontol Scand. 2019;77:457-467.
12. Puzio, M.; Błaszczyszyn, A.; Hadzik, J.; Dominiak, M. Puzio, M.; Błaszczyszyn, A.; Hadzik, J.; Dominiak, M. Ultrasound Assessment of Soft Tissue Augmentation around Implants in the Aesthetic Zone Using a Connective Tissue Graft and Xenogeneic Collagen Matrix—1-Year Randomised Follow-Up. Ann. Anat. Anat. Anz. 2018;217:129-141.
13. Thoma DS, Gasser TJW, Jung RE, Hämmerle CHF. Randomized controlled clinical trial comparing implant sites augmented with a volume-stable collagen matrix or an autogenous connective tissue graft: 3-year data after insertion of reconstructions. J Clin Periodontol. 2020;47:630-639.
14. Huang JP, Liu JM, Wu YM, Dai A, Hu HJ, He FM, Chen QM, Li XJ, Sun P, Ding PH. Clinical evaluation of xenogeneic collagen matrix versus free gingival grafts for keratinized mucosa augmentation around dental implants: A randomized controlled clinical trial. J Clin Periodontol. 2021;48:1293-1301.
15. Thoma DS, Buranawat B, Hämmerle CHF, Held U, Jung RE. Efficacy of soft tissue augmentation around dental implants and in partially edentulous areas: a systematic review. J Clin Periodontol. 2014;15:77-91.
16.Naenni N, Walter P, Hämmerle CHF, Jung RE. Augmentation of soft tissue volume at pontic sites: a comparison between a cross-linked and a non-cross-linked collagen matrix. Clin Oral Investig. 2021;25:1535-1545.
17. Thoma DS, M Zeltner, M Hilbe, Hämmerle CHF, Hüsler J, Jung RE. Randomized controlled clinical study evaluating effectiveness and safety of a volume-stable collagen matrix compared to autogenous connective tissue grafts for soft tissue augmentation at implant sites. J Clin Periodontol. 2016;43:874- 875.
18. Zucchelli G, Tavelli L, McGuire MK, Rasperini G, Feinberg SE, Wang HL, Giannobile WV. Autogenous soft tissue grafting for periodontal and peri-implant plastic surgical reconstruction. J Periodontol. 2020;91:9-16.
19. Tavelli L, Barootchi S, Vera Rodriguez M, Mancini L, Meneghetti PC, Mendonça G, Wang HL. Early soft tissue changes following implant placement with or without soft tissue augmentation using a xenogeneic cross-link collagen scaffold: A volumetric comparative study. J Esthet Restor Dent. 2022;34:181-187.
20. Puzio M, Hadzik J, Błaszczyszyn A, Gedrange T, Dominiak M. Soft tissue augmentation around dental implants with connective tissue graft (CTG) and xenogenic collagen matrix (XCM). 1-year randomized control trial. Ann Anat. 2020;230:151484.
21. Neumeyer S. Extrusionstherapie, Zahn prax 15, Sonderaus gaben Implantologie. 2012;20-25.
1. Angelis P, Manicone PF, Gasparini G, Angelis S, Liguori MG, Filippis I, D'Addona A. Influence of Immediate Implant Placement and Provisionalization with or without Soft Tissue Augmentation on Hard and Soft Tissues in the Esthetic Zone: A One-Year Retrospective Study. Biomed Res Int. 2021;2021:8822804.
2. Ashurko IP, Tarasenko SV, Esayan AV, Galyas AI, Li AV. Evaluation of free connective tissue graft and collagen matrix clinical effectiveness to increase soft tissue thickness around dental implants. Paradontology. 2022;27:2.
3. Bassetti M, Kaufmann R, Salvi GE, Sculean A, Bassetti R. Soft tissue grafting to improve the attached mucosa at dental implants: A review of the literature and proposal of a decision tree. Quintessence Int. 2015;46:499-510.
4. Burkhardt R, Hämmerle CHF, Lang NP, Research Group on Oral Soft Tissue Biology & Wound Healing. Self-reported pain perception of patients after mucosal graft harvesting in the palatal area. J Clin Periodontol. 2015;42:281-287.
5. Caballé-Serrano J, Zhang S, Ferrantino L, Simion M, Chappuis V, Bosshardt DD. Tissue Response to a Porous Collagen Matrix Used for Soft Tissue Augmentation. Materials (Basel). 2019;12:3721.
6. Gargallo-Albiol J, Barootchi S, Tavelli L, Wang HL. Efficacy of Xenogeneic Collagen Matrix to Augment Peri-Implant Soft Tissue Thickness Compared to Autogenous Connective Tissue Graft: A Systematic Review and Meta-Analysis. Int J Oral Maxillofac Implants. 2019;34:1059-1069.
7. Giannobile WV, Jung RE, Schwarz F, Groups of the 2nd Osteology Foundation Consensus Meeting. Evidence-based knowledge on the aesthetics and maintenance of peri-implant soft tissues: Osteology Foundation Consensus Report Part 1-Effects of soft tissue augmentation procedures on the maintenance of peri-implant soft tissue health. Clin Oral Implants Res. 2018;29:7-10.
8. Deo SD, Shetty SK, Kulloli A, Chavan R, Dholakia P, Ligade S, Dharmarajan G. Efficacy of free gingival graft in the treatment of Miller Class I and Class II localized gingival recessions: A systematic review. J Indian Soc Periodontol. 2019;23:93-99.
9. Zucchelli G. и др. Autogenous soft tissue grafting for periodontal and peri-implant plastic surgical reconstruction. J. Periodontol. 2020;91:9-16.
10. De Angelis P, De Angelis S, Passarelli PC, Liguori MG, Pompa G, Papi P, Manicone PF, D'Addona A. Clinical comparison of a xenogeneic collagen matrix versus subepithelial autogenous connective tissue graft for augmentation of soft tissue around implants. Int J Oral Maxillofac Surg. 2021;50:956- 963.
11. Moraschini V, de Almeida DCF, Sartoretto S, Bailly Guimarães H, Chaves Cavalcante I, Diuana Calasans-Maia M. Clinical efficacy of xenogeneic collagen matrix in the treatment of gingival recession: a systematic review and meta-analysis. Acta Odontol Scand. 2019;77:457-467.
12. Puzio, M.; Błaszczyszyn, A.; Hadzik, J.; Dominiak, M. Puzio, M.; Błaszczyszyn, A.; Hadzik, J.; Dominiak, M. Ultrasound Assessment of Soft Tissue Augmentation around Implants in the Aesthetic Zone Using a Connective Tissue Graft and Xenogeneic Collagen Matrix—1-Year Randomised Follow-Up. Ann. Anat. Anat. Anz. 2018;217:129-141.
13. Thoma DS, Gasser TJW, Jung RE, Hämmerle CHF. Randomized controlled clinical trial comparing implant sites augmented with a volume-stable collagen matrix or an autogenous connective tissue graft: 3-year data after insertion of reconstructions. J Clin Periodontol. 2020;47:630-639.
14. Huang JP, Liu JM, Wu YM, Dai A, Hu HJ, He FM, Chen QM, Li XJ, Sun P, Ding PH. Clinical evaluation of xenogeneic collagen matrix versus free gingival grafts for keratinized mucosa augmentation around dental implants: A randomized controlled clinical trial. J Clin Periodontol. 2021;48:1293-1301.
15. Thoma DS, Buranawat B, Hämmerle CHF, Held U, Jung RE. Efficacy of soft tissue augmentation around dental implants and in partially edentulous areas: a systematic review. J Clin Periodontol. 2014;15:77-91.
16.Naenni N, Walter P, Hämmerle CHF, Jung RE. Augmentation of soft tissue volume at pontic sites: a comparison between a cross-linked and a non-cross-linked collagen matrix. Clin Oral Investig. 2021;25:1535-1545.
17. Thoma DS, M Zeltner, M Hilbe, Hämmerle CHF, Hüsler J, Jung RE. Randomized controlled clinical study evaluating effectiveness and safety of a volume-stable collagen matrix compared to autogenous connective tissue grafts for soft tissue augmentation at implant sites. J Clin Periodontol. 2016;43:874- 875.
18. Zucchelli G, Tavelli L, McGuire MK, Rasperini G, Feinberg SE, Wang HL, Giannobile WV. Autogenous soft tissue grafting for periodontal and peri-implant plastic surgical reconstruction. J Periodontol. 2020;91:9-16.
19. Tavelli L, Barootchi S, Vera Rodriguez M, Mancini L, Meneghetti PC, Mendonça G, Wang HL. Early soft tissue changes following implant placement with or without soft tissue augmentation using a xenogeneic cross-link collagen scaffold: A volumetric comparative study. J Esthet Restor Dent. 2022;34:181-187.
20. Puzio M, Hadzik J, Błaszczyszyn A, Gedrange T, Dominiak M. Soft tissue augmentation around dental implants with connective tissue graft (CTG) and xenogenic collagen matrix (XCM). 1-year randomized control trial. Ann Anat. 2020;230:151484.
21. Neumeyer S. Extrusionstherapie, Zahn prax 15, Sonderaus gaben Implantologie. 2012;20-25.